It is with great sadness that we report that Dr. Michael Cahalan has passed away, after battling AML for several months.
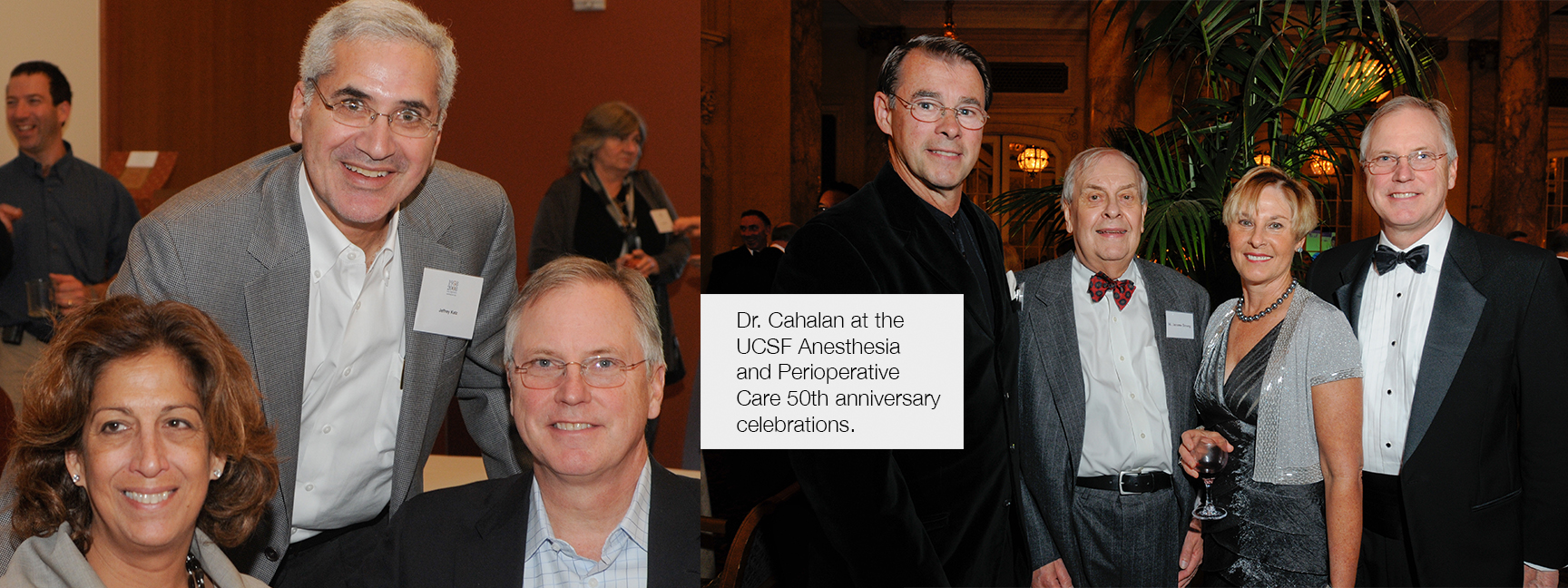
Dr. Cahalan was a long-time member of the UCSF Anesthesia and Perioperative Care Department, starting in residency (he was the chief resident, Class of 1978), followed by a fellowship with Ted Eger (1978-1979) and then joining the faculty (1979). He was Chief of Cardiac Anesthesia at UCSF for 22 years, and was the 1985 recipient of the William K. Hamilton Award for Excellence in Teaching. He was a giant in our specialty, performing the first perioperative TEE while Chief of Cardiac Anesthesia at UCSF (read more below). He then went on to a highly successful career as Chair of Anesthesia at the University of Utah, serving in this role for 15 years, until his death.
He had a great impact on many careers, including that of UCSF Anesthesia Chair Michael Gropper. Those that knew him will remember his deep commitment to his patients, our specialty, the trainees, his colleagues, and especially his wife Marianne. He had a quick wit and warm personality, always taking the time to support all that he met. He will be greatly missed.
A Fundamentally Better Way to Monitor Patients
One day in the early 1990’s, in the Moffit OR suite, Ron Miller rushed down the hall and said to his colleague Michael Cahalan: “We’re losing this patient; come take a look.”
When they arrived, Miller showed Cahalan a septic woman whose heart rate was 150 beats per minute and systolic arterial blood pressure was 50 mmHg. Miller explained that they had already given the woman appropriate amounts of blood and still did not know whether the problem was hypo- or hypervolemia. Cahalan, an expert in transesophageal echocardiography (TEE), put a scope down the woman’s throat, revealing a nearly empty heart. After they administered the appropriate fluids intravenously, arterial blood pressure increased and the heart slowed. The procedure, known as rescue echo, is rapidly becoming the standard for life-threatening hypotension. It also was the culmination of a clinical research path that Cahalan had begun a decade or so before.
In 1981, Cahalan was an assistant professor working in the Eger lab when Bill Hamilton asked him to meet with a new cardiology fellow named Peter Kramer. Under the tutelage of Nelson Schiller and in collaboration with an outside engineer, Cahalan and Kramer began working with mini-ultrasound transducers mounted on a gastroscope in an effort to obtain improved pictures of the heart. Within months, three groups around the world received permission to begin testing the devices – now with two-dimensional transducers – on human subjects. Cahalan, Kramer, Schiller, and Mike Roizen received their first 2-D device in late 1981, while working in Moffit’s OR-10.
“We slipped the scope down and suddenly, in real time, saw a moving image of all four chambers of the heart,” said Cahalan. “My jaw hit the ground and I knew right away this was a fundamentally better way to monitor patients.”
Over the next couple of years, UCSF fellows demonstrated how TEE provided a much more accurate measure of ventricular filling than traditional measures of ischemia. Meanwhile, the purchase of a 19’’ black and white monitor for the OR proved to be a critical “epiphany for the cardio and vascular surgeons, who saw that this could answer important questions about clinical care,” said Cahalan. Their support proved crucial, as initially TEE was considered dangerous and the papers about it were widely rejected. When Cahalan returned to UCSF in 1986, after a sabbatical in Europe, it was the surgeons’ support that convinced the hospital to purchase the first commercial edition of the device.
As chair at the University of Utah in 2008, Cahalan sat on a committee that recommended TEE for monitoring during all cardiac procedures. Anesthesiologists and surgeons at UCSF had understood its importance 25 years ahead of the curve.