Cardiac Catheterization Lab Procedures- PCI and Beyond
Moving Beyond PCI-Complex Cardiac Catheterization Procedures
- Percutaneous Coronary Intervention
- First PCI performed in 1977 in by Dr. Gruentzig in Zurich, Switzerland
- Cases initally performed by cardiac anesthesia with surgical room on standby (First CABG performed in 1961)
- Now performed 97% with nursing sedation at UCSF
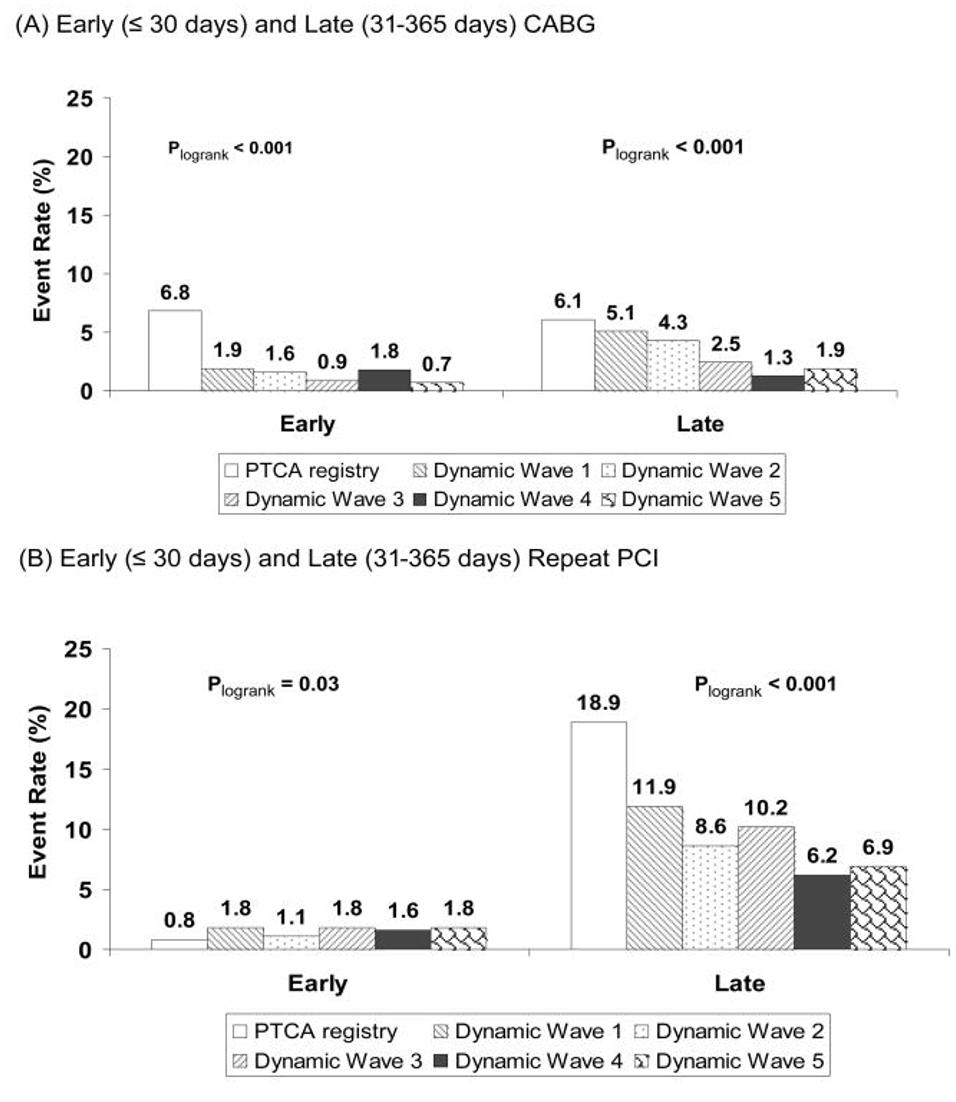
4.Venkitachalam L et al.;Investigators of NHLBI-Sponsored 1985-1986 PTCA and 1997-2006 Dynamic Registries. Twenty-year evolution of percutaneous coronary intervention and its impact on clinical outcomes: a report from the National Heart, Lung, and Blood Institute-sponsored, multicenter 1985-1986 PTCA and 1997-2006 Dynamic Registries. Circ Cardiovasc Interv. 2009 Feb;2(1):6-13.
Anesthesia for Chronic Total Occlusion (CTO) PCI
- Defined as any vessel with >3 months of total occlusion
- First CTO PCI was performed in 1990 by Dr. Kahn
- Procedural success now approaches 90%
- CTO PCI has been shown to improve quality of life and reduce angina compared to medical therapy alone [5]
- These procedures are technically challenging, with a prolonged procedure time and an increased risk of complications compared to standard PCI
- Rotary drills, lasers, and multiple stents may be used, which are associated with increased rate of procedure complexity, time, and complication rate
- Performed 56 of these in 2022 at UCSF last year
5.Gerald S Werner and others, A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions, European Heart Journal, Volume 39, Issue 26, 07 July 2018, Pages 2484–2493
Approaches to Chronic Total Occlusion (CTO) PCI
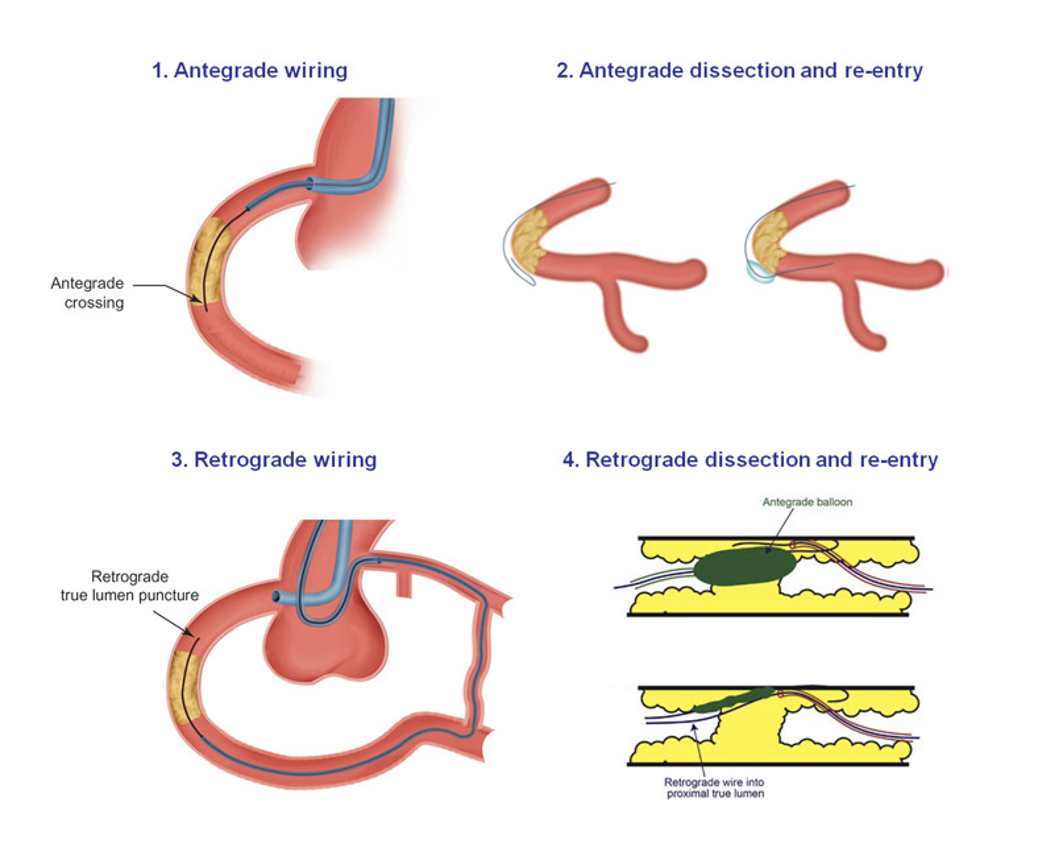
6.Brilakis ES. Manual of Coronary Chronic Total Occlusion Interventions. A Step-By-Step Approach. 2nd edition: Elsevier; 2017.
Mechanical Support Devices for CTO PCI
- Mechanical assist devices may be used (IABP, ECLS, or Impella) either prophylactically or for rescue shock
- Consult with cardiac anesthesiologist on call for support on these cases, there is now a protocol on anesthesia intranet
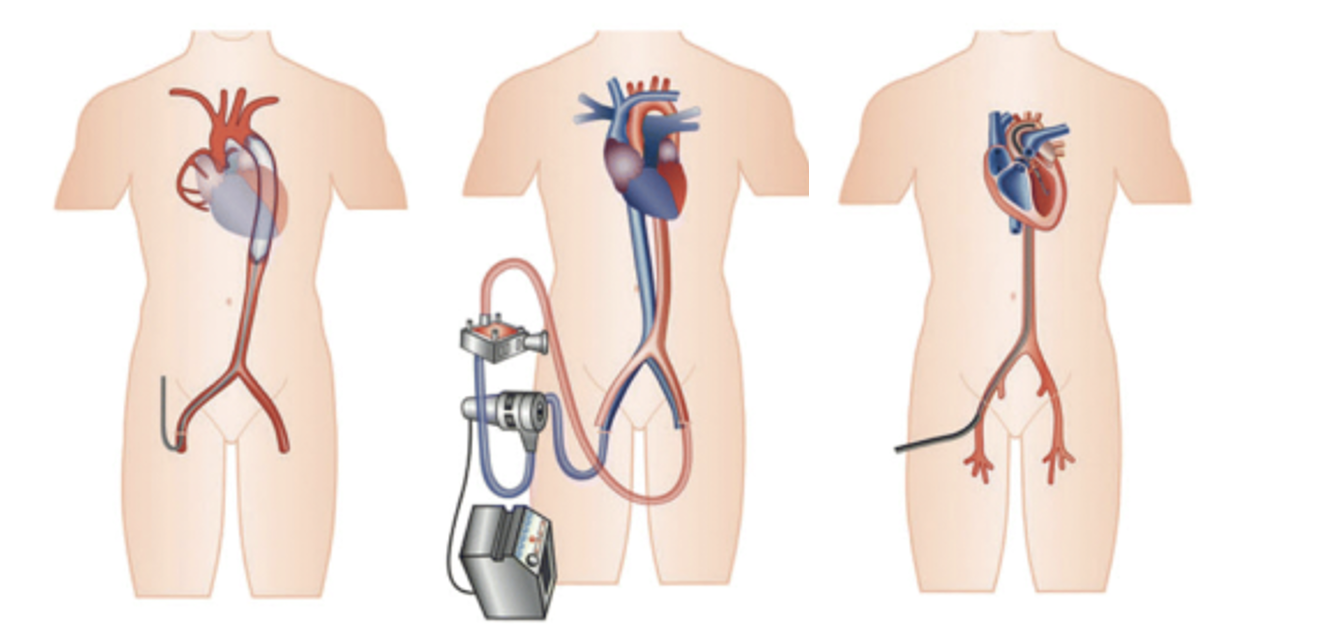
6.Brilakis ES. Manual of Coronary Chronic Total Occlusion Interventions. A Step-By-Step Approach. 2nd edition: Elsevier;. 2017
Anesthesia for Chronic Total Occlusion (CTO) PCI
- Clinical pearls can be found on anesthesia intranet
- Radial access is often too small to deliver the requisite catheters and guidewires hence bifemoral access is common
- Patients should be given preop DAPT if they can tolerate
- Cross matched blood should be available
- Anesthetic goals should be similar to PCI with understanding of length (3-5 hrs) and potential complications
- Either GA or sedation is appropriate depending on patient, no studies to support either
- There are recommendations for particularly difficult lesions to favor GA to facilitate immobility and procedural success
- Any drugs for maintenance of anesthesia are appropriate
- Heparinization is requested during the procedure to keep ACT >300s
- Standard monitors + invasive arterial pressure should be transduced, and femoral sheath transduction can be requested of cardiologists
- Central venous femoral access can be requested as well
- Vasoactive drugs should be chosen in collaboration with cardiology team to facilitate procedure and minimize complications
- Defibrillator pads should be placed to manage arrythmias
- Most common procedural complications during CTO PCI
- Coronary artery perforation (4-6%)
- Access site complications
- Myocardial ischemia
- Coronary vessel dissection or thromboembolism
- Pericardial effusion (2-3%)
- Tamponade (1-2%) requiring pericardial drain by cardiologists
- Transient rhythm issues (Sinus Bradycardia or small runs of VT)
- All present as undifferentiated hypotension so it’s important to have clear communication with cardiologist
- What did you do last?
- What do you see on fluoroscopy?
Anesthesia for Mitraclip Procedures
Mitraclip is a percutaneous device that provides edge to edge approximation of mitral leaflets for severe mitral regurgitation 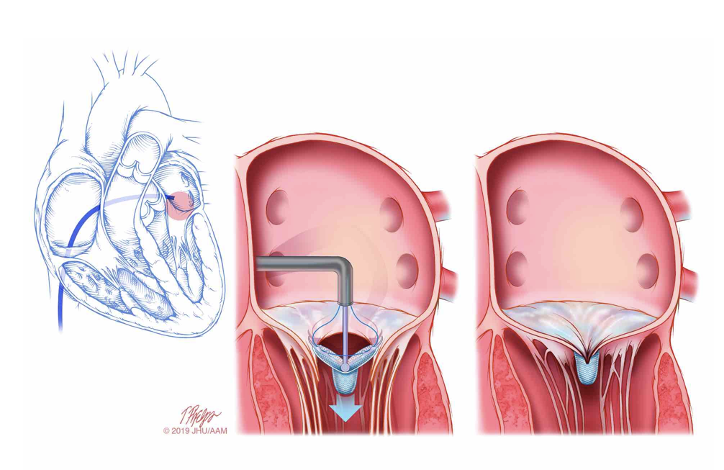
- Shows improvement in left ventricular size, New York Heart Association functional class, and quality-of-life measures
- Performed 88 of these in 2022 at UCSF
- Two types of patients:
- Those delaying surgical valves
- Those who are high risk operative risk
- Clinical pearls can be found on intranet
- GA with ETT +arterial line (usually placed by us but can ask cards for fem sheath preprocedure)
- Commonly high doses of inotropes and vasoconstrictors needed
- Particularly in setting of lowered EF with severe MR
- Not much stimulation post induction
- Left atrial pressure can be transduced to help guide your volume management
- Cardiology TEE team can assess function and volume
- May ask for lower intraoperative tidal volumes and high PEEP to reduce movement effect of respiration on heart
- Helpful to keep patients paralyzed
- Heparinization requested once transseptal puncture
- Small risk of pericardiac effusion
- TEE team can diagnose and Interventional Cards can drain
- Rarely mitral regurgitation is traded for mitral stenosis as clips are applied
- Usually the postinduction inotropes and vasoconstrictors can be weaned during wakeup
- Most can be extubated and recover in PACU
- Occasionally require ICU admission for continuing inotropic needs or pericardial drain
Anesthesia for TAVR Procedures
Transcatheter Aortic Valve Replacement (TAVR)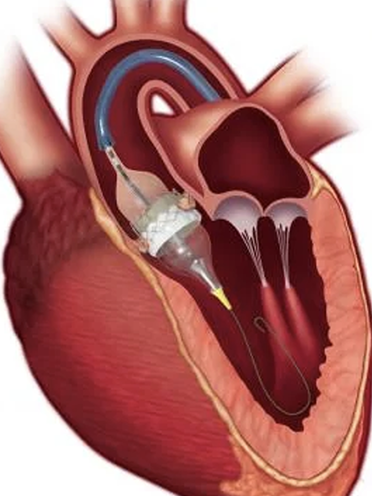
- First TAVR performed in 2002 by Dr. Cribier in Rouen, France
- Initially FDA approved in 2010 for nonoperative AS candidates (Partner I)
- In 2019 FDA approved for low risk surgical candidates as well (Partner III)
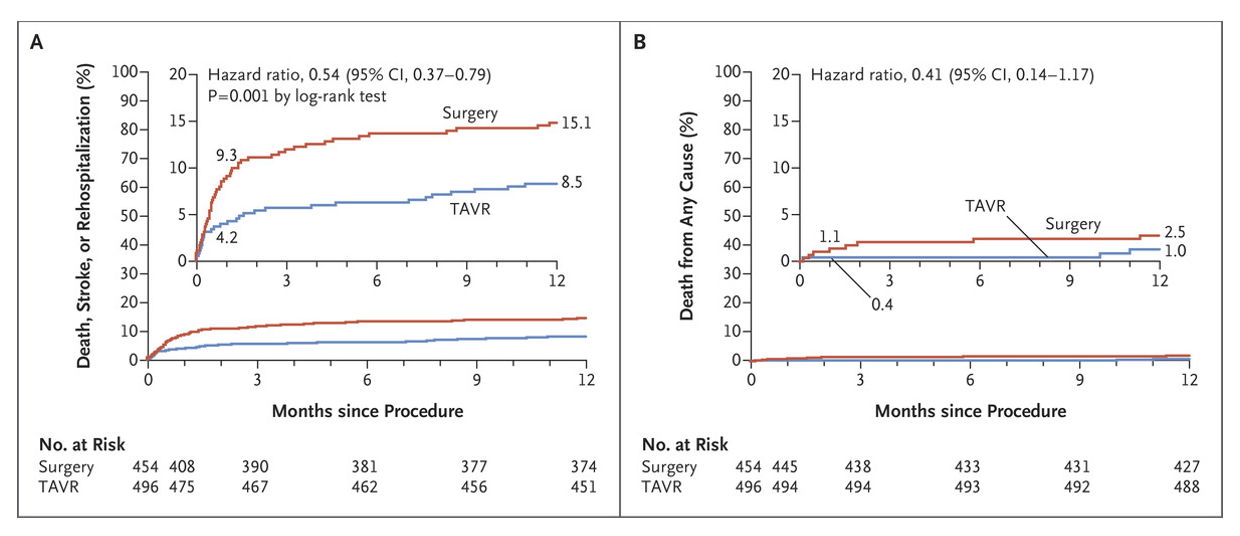
- Partner III Trial [7] showed that TAVRs in low risk patients
- Lower rate of stroke than surgery (P=0.02)
- Lower rates of death (P=0.01)
- Lower rate of atrial fibrillation (P<0.001).
- Shorter index hospitalization than surgery (P<0.001)
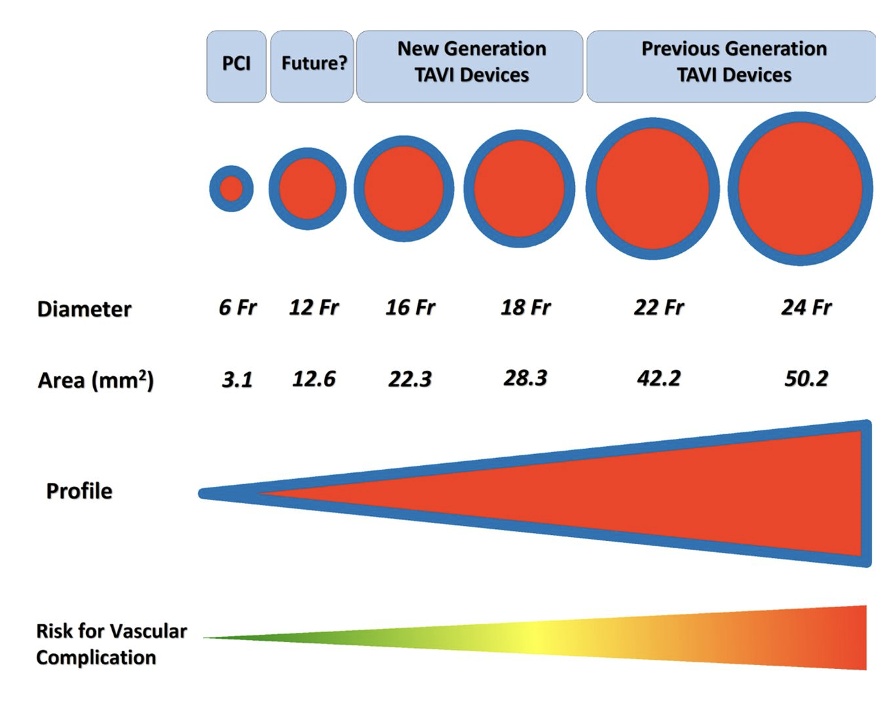
- Risks of vessel injury have dramatically reduced from the initial sheaths (24Fr/8mm) to the most recent generations of insertion sheaths (14 Fr e-sheaths/4.7mm)
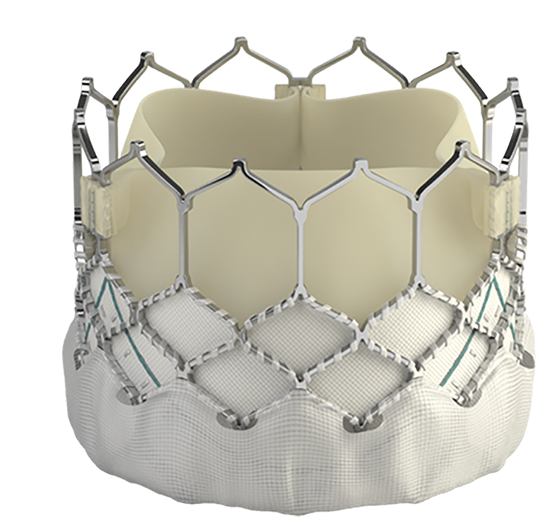
- Newest valves have skirts designed to reduce paravalvarleak and requiring less balloon dilation of valve, and thus reducing risk of disruption to aorta and long term aortic insufficiency
- Now routinely being guided by angiography and TTE
- Studies have begun to report to show that patients undergoing sedation for TAVR have improved outcomes compared to general anesthesia [8-9]
- Lower 30-day mortality (2.9% vs. 4.1%, p=0.029)
- Lower composite mortality and/or stroke rate (4.8% vs. 6.4%, p=0.019)
- Shorter hospital length of stay (6 d vs. 6.7 d, p<0.0001)
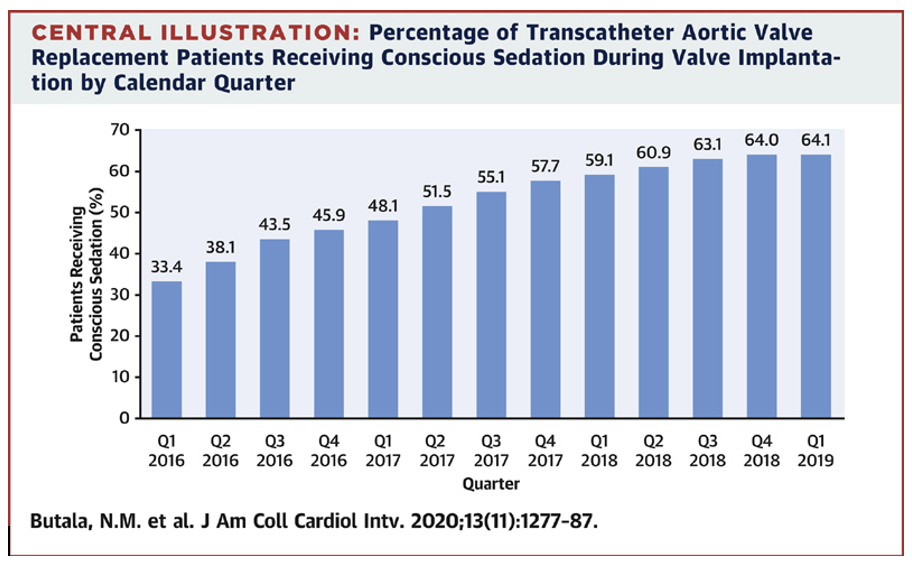
8.Fröhlich GM, Lansky AJ, Webb J, Roffi M, Toggweiler S, Reinthaler M. et al. Local versus general anesthesia for transcatheter aortic valve implantation (TAVR)--systematic review and meta-analysis. BMC Med. 2014;12:41. 9.
9.N Butala , et al. Conscious Sedation Versus General Anesthesia for Transcatheter Aortic Valve Replacement: Variation in Practice and Outcomes.
Am Coll Cardiol Intv. 2020 Jun, 13 (11) 1277–1287.
- Large centers, particularly in Europe, now perform nursing sedation for many TAVRs [10-11] in Cath lab
- Emory recently reported on their experience where ~50% of their patients now get nursing sedation [10]
- Improved satisfaction, improved scheduling flexibility, decreased resource utilization [10]
10.Patricia Keegan et al. (2020): Nurse Led Sedation: The Clinical and Echocardiographic Outcomes of the 5-Year Emory Experience, Structural Heart. May 27 2020.
11.Browne Suzy et al. Evaluation of nurse- and anaesthetist-led sedation for selected transcatheter aortic valve implantation procedures British Journal of Cardiac Nursing 2022 87:11, 1-9
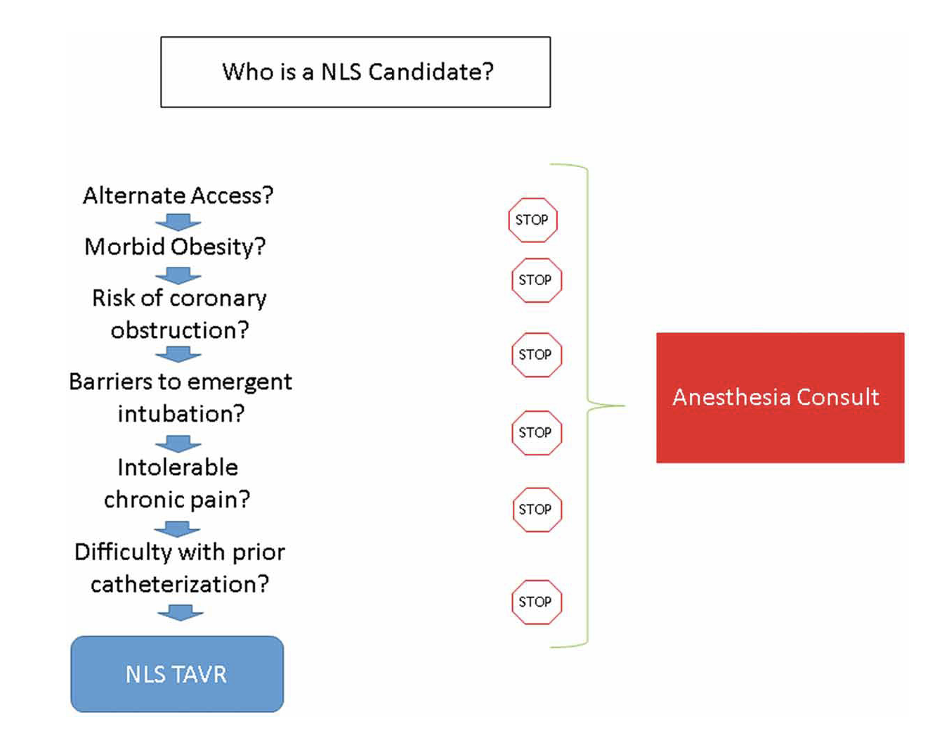
- 88% of TAVRs at UCSF are performed under MAC sedation
- Select TAVRs at UCSF no longer have the support of cardiac surgery, perfusion, and cardiothoracic nursing
- For now still have cardiac anesthesia
- Transition suggests some TAVRs will move to Cath lab
- What is optimal anesthesia resource utilization?
- Cardiac anesthesia vs Anesthesia support vs Nursing sedation?
- Is a cardiologist and a sedation nurse better than an anesthesiologist?
- Debated at 2021 ASA Conference: “Anesthetic Management for TAVR: Too Much, Too Little, or Stuck in the Middle?”
- Expect to hear this debate at UCSF in coming years
- Expect we will still be called for “complicated” sedations and complex interventions
This information is meant to serve as an educational resource. Clinicians should use their own professional judgment in the care of any individual patient as the guidance contained in this document may not be appropriate for all patients or all situations.