Lee Lab
Welcome to the Lee Lab
For the past several years, my research has focused on the mechanisms by which mesenchymal stem cells (MSC) may normalize alveolar epithelial permeability and fluid transport in animal and human models of acute lung injury (ALI), including a novel ex vivo perfused human lung preparation injured by endotoxin or bacteria, in collaboration with Michael Matthay, MD.
More recently, my laboratory has begun studying the roles of microvesicles (MVs) released by both embryonic and adult stem cells in lung injury and cancer as a possible therapeutic and as an alternative to the stem cells themselves. MVs are circular membrane fragments (50-200 nM in size) released from endosomal compartment as exosomes or shed from the surface membranes, which retain the phenotype of the cells from which they originate. In various models of injury, MSC MVs, through surface receptors, homed to the site of inflammation and interacted with the injured epithelium or endothelium through transfer of mRNA, microRNA, protein, receptor and/or organelle.
Major Goals: To understand (1) the mechanisms how microvesicles are formed by stem cells, (2) how pre-conditioning the stem cells can change the phenotype of the released microvesicles and (3) whether the therapeutic potency of the microvesicles can be enhanced using various models of lung injury or cancer.
Funding Sources: NIH NHLBI, Hamilton Endowment Funds (UCSF Department of Anesthesiology), UCSF RAP Grant.
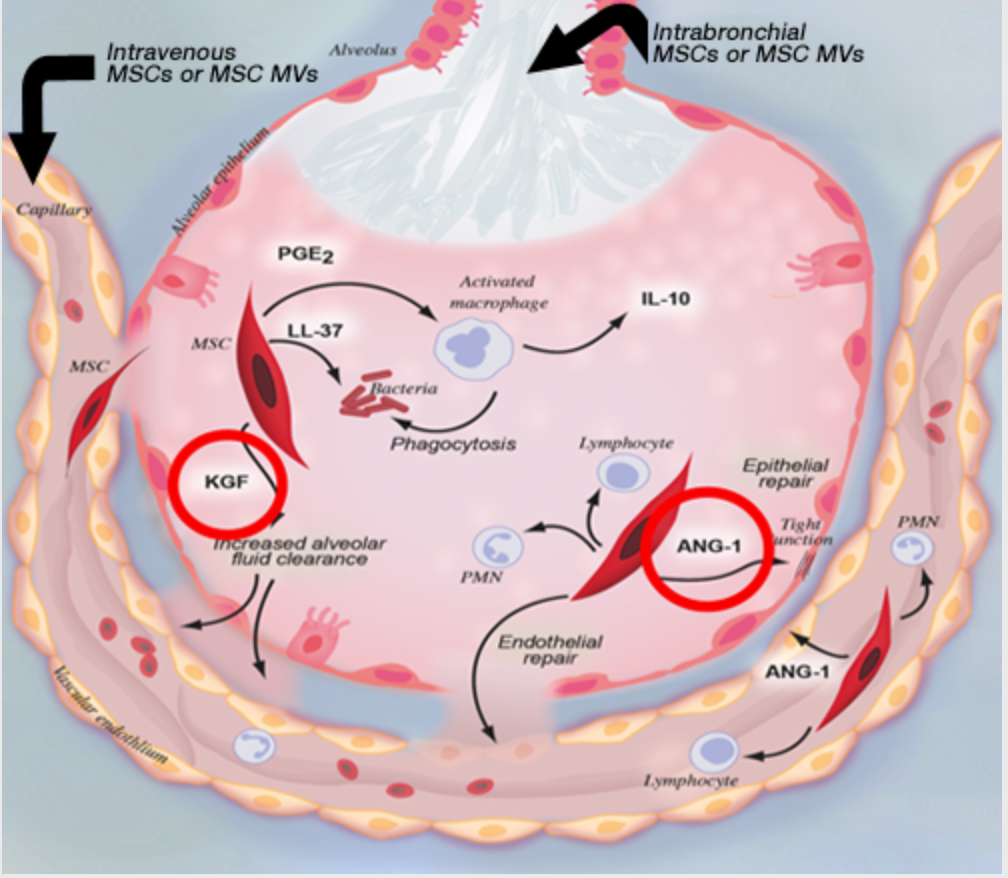 Underlying Mechanisms of MSC Based Therapy for Acute Lung Injury. In acute lung injury, the therapeutic properties of MSC rely on both a paracrine mechanism and through interaction with other cells. Multiple mechanisms have been identified through which MSC therapy may repair the alveolar epithelium and endothelium during acute lung injury such as (1) secretion of paracrine soluble factors which restore alveolar fluid clearance, lung permeability and inhibit bacterial growth and (2) immunomodulation of innate and adaptive immune cells which reduce alveolar inflammation. Although not fully characterized, the potential of engraftment by in vivo modified MSC and the presence of endogenous adult stem cells with characteristics similar to MSC may also contribute to this therapeutic effect. (Figure made by Diana Lim. Published in Lee et al. Stem Cells 29(6): 913-919, 2011)
Underlying Mechanisms of MSC Based Therapy for Acute Lung Injury. In acute lung injury, the therapeutic properties of MSC rely on both a paracrine mechanism and through interaction with other cells. Multiple mechanisms have been identified through which MSC therapy may repair the alveolar epithelium and endothelium during acute lung injury such as (1) secretion of paracrine soluble factors which restore alveolar fluid clearance, lung permeability and inhibit bacterial growth and (2) immunomodulation of innate and adaptive immune cells which reduce alveolar inflammation. Although not fully characterized, the potential of engraftment by in vivo modified MSC and the presence of endogenous adult stem cells with characteristics similar to MSC may also contribute to this therapeutic effect. (Figure made by Diana Lim. Published in Lee et al. Stem Cells 29(6): 913-919, 2011)
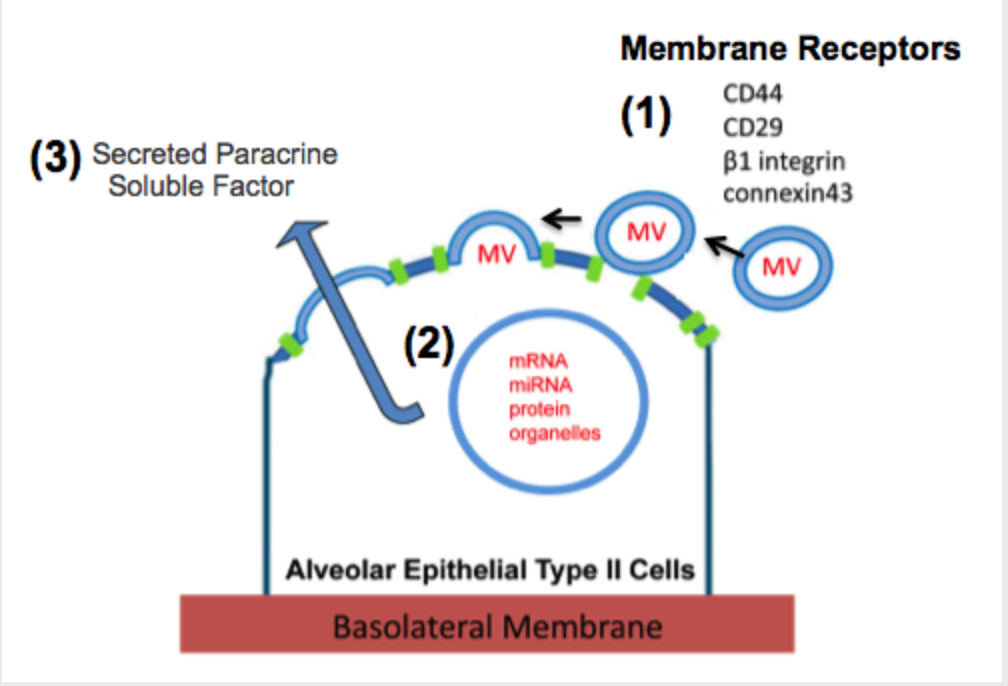 Potential Mechanisms Underlying the Therapeutic Effect of Microvesicles Released by Mesenchymal Stem Cells. During acute lung injury, MSC MVs are targeted towards the injured alveolar epithelium by surface receptors, such as possibly CD44 or CD29 or through connexin 43 channels, leading to the endocytosis of its contents, which includes mRNA, miRNA, proteins and organelle. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
Potential Mechanisms Underlying the Therapeutic Effect of Microvesicles Released by Mesenchymal Stem Cells. During acute lung injury, MSC MVs are targeted towards the injured alveolar epithelium by surface receptors, such as possibly CD44 or CD29 or through connexin 43 channels, leading to the endocytosis of its contents, which includes mRNA, miRNA, proteins and organelle. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
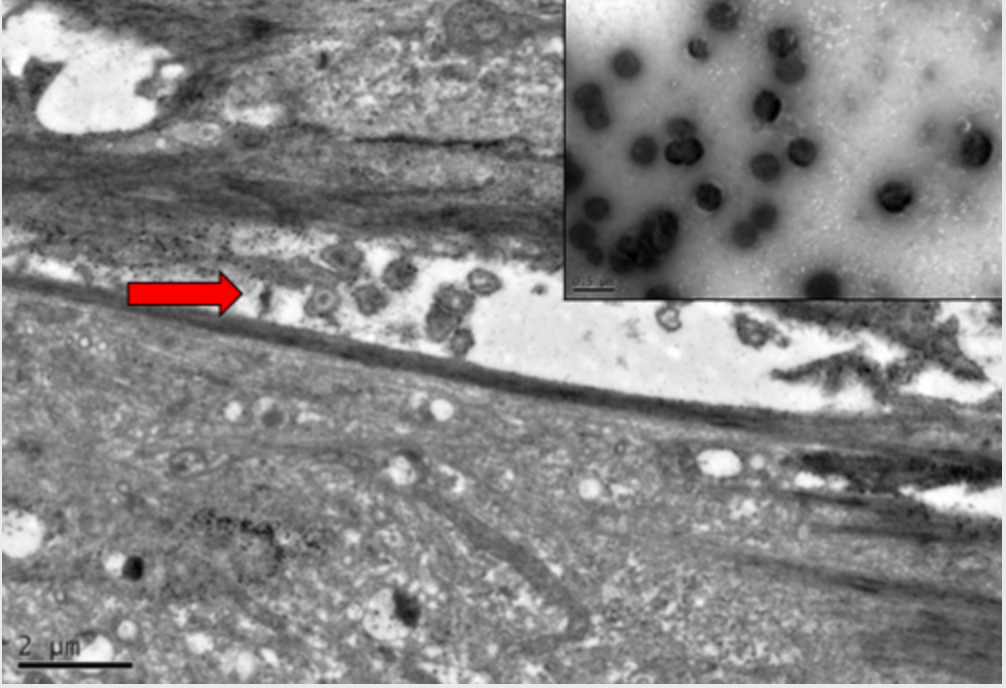 Electron Microscopy Images of MVs Released by MSCs. Electron microscopy demonstrates that MVs are released by MSCs in vitro following stress such as serum starvation. MVs released into the inter-cellular gap separating two MSCs; bar is 2μm. Enclosed image shows purified MVs, which appears to be a collection of homogeneous spheroids; bar is 0.5μm. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
Electron Microscopy Images of MVs Released by MSCs. Electron microscopy demonstrates that MVs are released by MSCs in vitro following stress such as serum starvation. MVs released into the inter-cellular gap separating two MSCs; bar is 2μm. Enclosed image shows purified MVs, which appears to be a collection of homogeneous spheroids; bar is 0.5μm. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
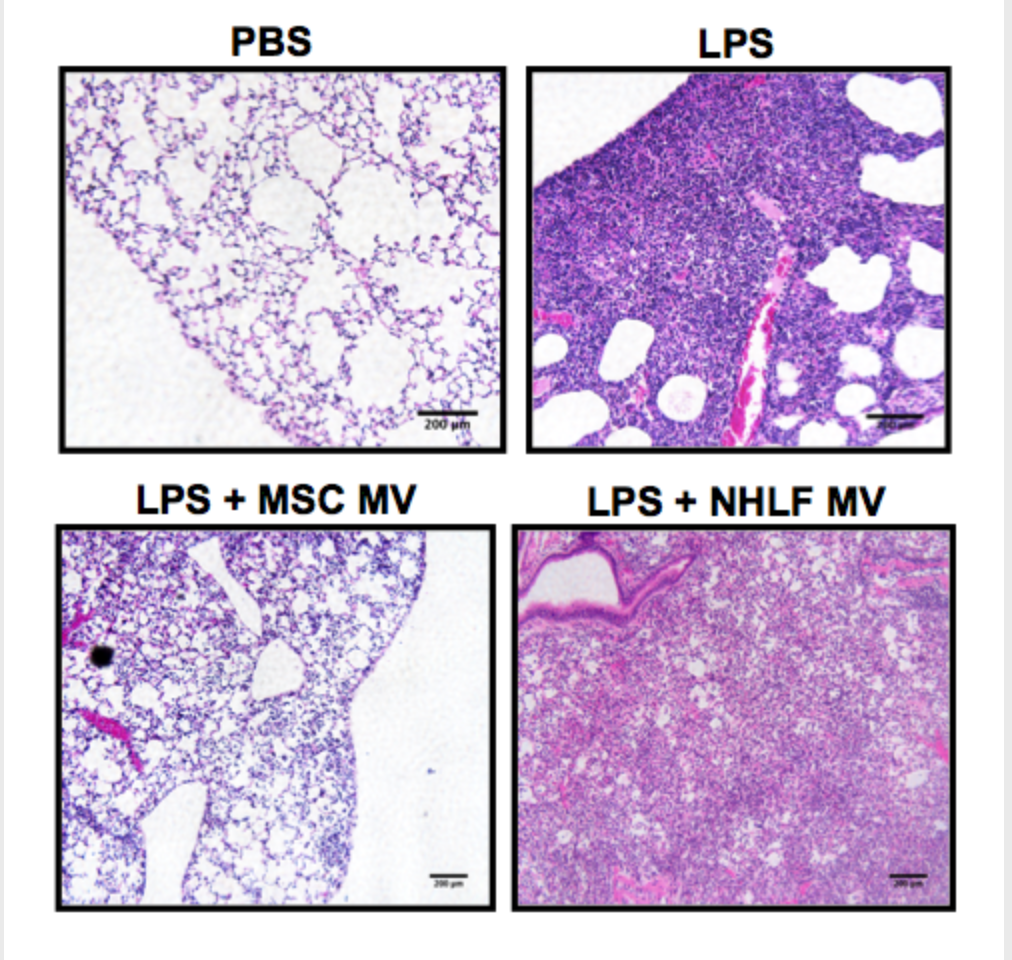 Effect of MSC MVs on Influx of Inflammatory Cells in Endotoxin-Induced ALI in Mice. The administration of MSC MVs reduced the influx of inflammatory cells in endotoxin-induced ALI in mice. IT MSC MVs improved lung injury as assessed by histology. H&E staining of lung sections at 48 h demonstrated a reduction in inflammatory cell influx, edema, blood and thickening of the interstitium in endotoxin-injured lungs treated with MSC MVs. The MVs derived from NHLF showed no therapeutic benefit on lung injury. Images are 10x magnification. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
Effect of MSC MVs on Influx of Inflammatory Cells in Endotoxin-Induced ALI in Mice. The administration of MSC MVs reduced the influx of inflammatory cells in endotoxin-induced ALI in mice. IT MSC MVs improved lung injury as assessed by histology. H&E staining of lung sections at 48 h demonstrated a reduction in inflammatory cell influx, edema, blood and thickening of the interstitium in endotoxin-injured lungs treated with MSC MVs. The MVs derived from NHLF showed no therapeutic benefit on lung injury. Images are 10x magnification. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
Therapeutic use of microvesicles released by mesenchymal stem cells in bacterial pneumonia-induced acute lung injury, using both animal and human models.
Therapeutic use of conditioned medium or microvesicles released by mesenchymal stem cells in hypoxia/ischemia induced injury in a model of neonatal asphyxia.
Therapeutic use of microvesicles released by pre-conditioned mesenchymal stem cells in breast cancer with lung metastases.
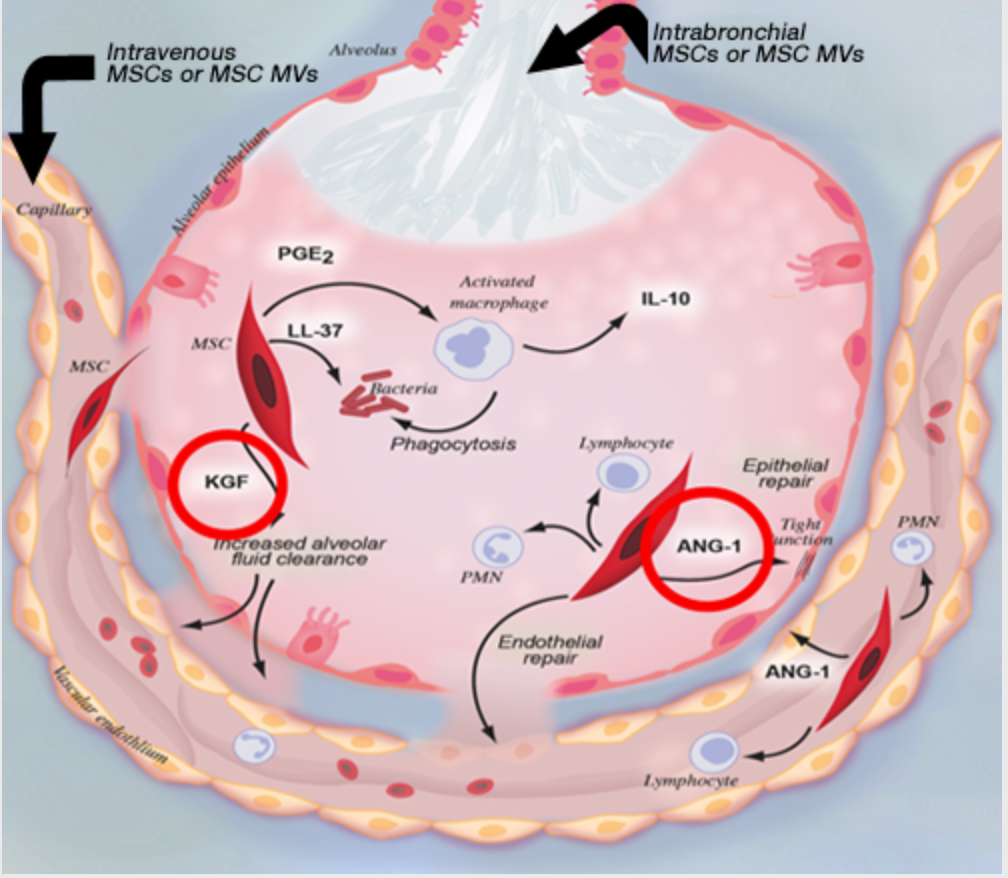 Underlying Mechanisms of MSC Based Therapy for Acute Lung Injury. In acute lung injury, the therapeutic properties of MSC rely on both a paracrine mechanism and through interaction with other cells. Multiple mechanisms have been identified through which MSC therapy may repair the alveolar epithelium and endothelium during acute lung injury such as (1) secretion of paracrine soluble factors which restore alveolar fluid clearance, lung permeability and inhibit bacterial growth and (2) immunomodulation of innate and adaptive immune cells which reduce alveolar inflammation. Although not fully characterized, the potential of engraftment by in vivo modified MSC and the presence of endogenous adult stem cells with characteristics similar to MSC may also contribute to this therapeutic effect. (Figure made by Diana Lim. Published in Lee et al. Stem Cells 29(6): 913-919, 2011)
Underlying Mechanisms of MSC Based Therapy for Acute Lung Injury. In acute lung injury, the therapeutic properties of MSC rely on both a paracrine mechanism and through interaction with other cells. Multiple mechanisms have been identified through which MSC therapy may repair the alveolar epithelium and endothelium during acute lung injury such as (1) secretion of paracrine soluble factors which restore alveolar fluid clearance, lung permeability and inhibit bacterial growth and (2) immunomodulation of innate and adaptive immune cells which reduce alveolar inflammation. Although not fully characterized, the potential of engraftment by in vivo modified MSC and the presence of endogenous adult stem cells with characteristics similar to MSC may also contribute to this therapeutic effect. (Figure made by Diana Lim. Published in Lee et al. Stem Cells 29(6): 913-919, 2011)
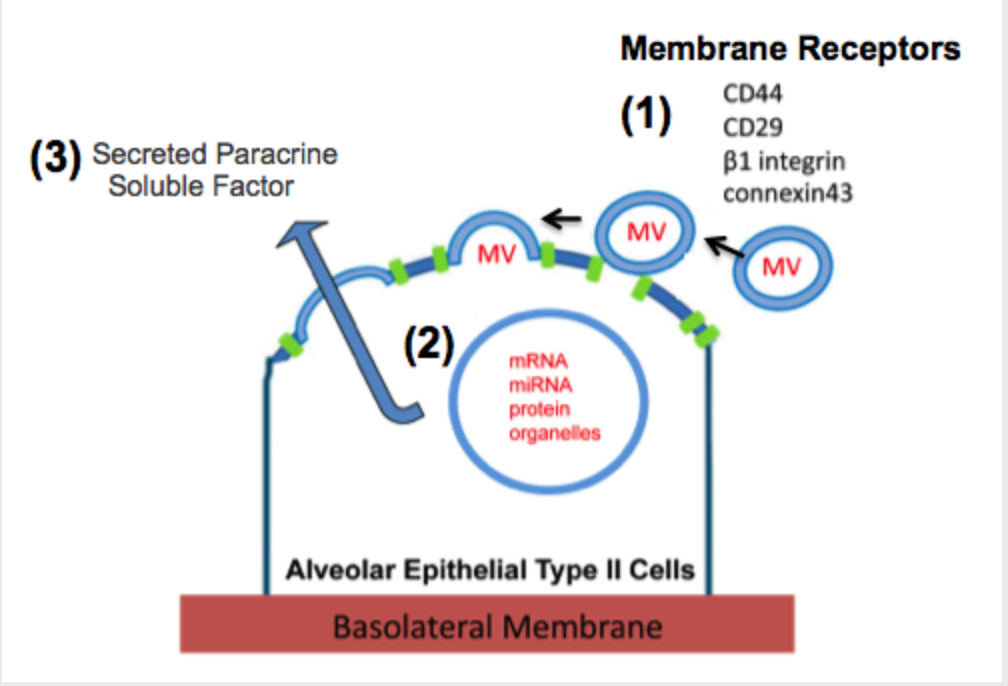 Potential Mechanisms Underlying the Therapeutic Effect of Microvesicles Released by Mesenchymal Stem Cells. During acute lung injury, MSC MVs are targeted towards the injured alveolar epithelium by surface receptors, such as possibly CD44 or CD29 or through connexin 43 channels, leading to the endocytosis of its contents, which includes mRNA, miRNA, proteins and organelle. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
Potential Mechanisms Underlying the Therapeutic Effect of Microvesicles Released by Mesenchymal Stem Cells. During acute lung injury, MSC MVs are targeted towards the injured alveolar epithelium by surface receptors, such as possibly CD44 or CD29 or through connexin 43 channels, leading to the endocytosis of its contents, which includes mRNA, miRNA, proteins and organelle. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
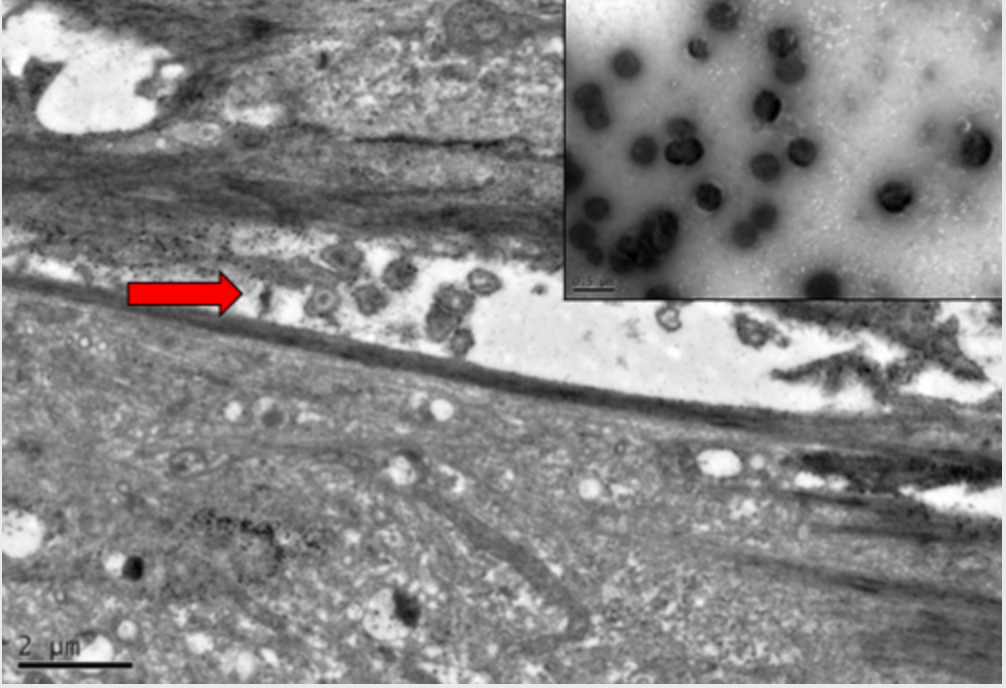
Electron Microscopy Images of MVs Released by MSCs. Electron microscopy demonstrates that MVs are released by MSCs in vitro following stress such as serum starvation. MVs released into the inter-cellular gap separating two MSCs; bar is 2μm. Enclosed image shows purified MVs, which appears to be a collection of homogeneous spheroids; bar is 0.5μm. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
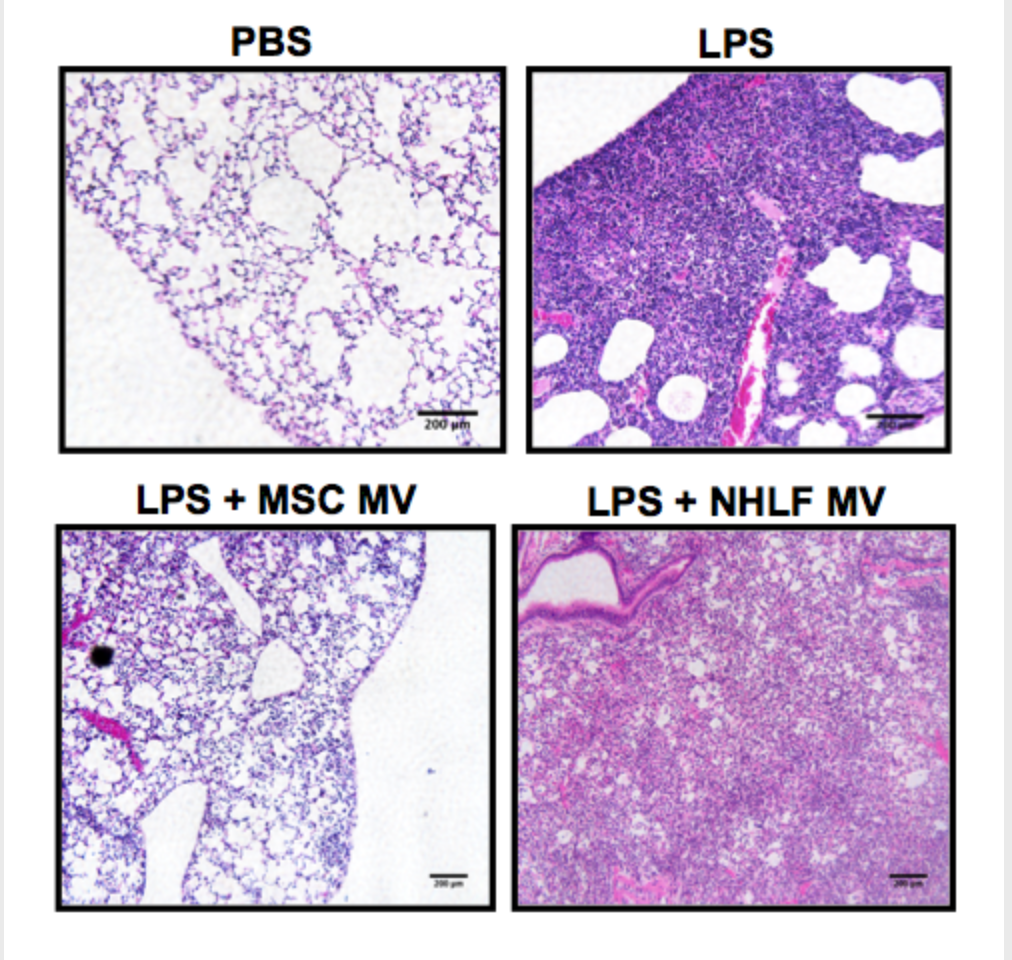 Effect of MSC MVs on Influx of Inflammatory Cells in Endotoxin-Induced ALI in Mice. The administration of MSC MVs reduced the influx of inflammatory cells in endotoxin-induced ALI in mice. IT MSC MVs improved lung injury as assessed by histology. H&E staining of lung sections at 48 h demonstrated a reduction in inflammatory cell influx, edema, blood and thickening of the interstitium in endotoxin-injured lungs treated with MSC MVs. The MVs derived from NHLF showed no therapeutic benefit on lung injury. Images are 10x magnification. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
Effect of MSC MVs on Influx of Inflammatory Cells in Endotoxin-Induced ALI in Mice. The administration of MSC MVs reduced the influx of inflammatory cells in endotoxin-induced ALI in mice. IT MSC MVs improved lung injury as assessed by histology. H&E staining of lung sections at 48 h demonstrated a reduction in inflammatory cell influx, edema, blood and thickening of the interstitium in endotoxin-injured lungs treated with MSC MVs. The MVs derived from NHLF showed no therapeutic benefit on lung injury. Images are 10x magnification. (Published in Zhu et al. Stem Cells 32(1):116-25, 2014)
Publications (2014-2022)
Manuscripts
- Zhu, YY, Feng, XM, Abbott, J, Fang, X, Hao, Q, Monsel, A, Qu, JM, Matthay, M, and Lee, JW. Human mesenchymal stem cell microvesicles for treatment of E.coli endotoxin induced acute lung injury in mice. Stem Cells 32(1):116-25, 2014. Article selected for F1000Prime.
- Ware, LB, Landeck, M, Koyama, T, Zhao, Z, Singer, J, Kern, R, Johnson, E, Janz, DR, Bernard, GR, Lee, JW, Matthay, MA, and the California Transplant Donor Network. A Randomized Trial of Nebulized Albuterol to Enhance Resolution of Pulmonary Edema in 506 Brain Dead Organ Donors. Am J Transplant 14(3):621-8, 2014.
- McAuley, DF, Curley, GF, Hamid, UI, Laffey, JG, Abbott, A, McKenna, DH, Fang, X, Matthay, MA, and Lee, JW. Clinical Grade Allogeneic Human Mesenchymal Stem Cells Restore Alveolar Fluid Clearance in part through a KGF-dependent mechanism in Human Lungs Rejected for Transplantation. Am J Physiol Lung Cell Mol Physiol 306(9):L809-15, 2014. Article was selected for APSselect, an acknowledgement of the best of recent submissions to the American Physiological Society journals.
- Asmussen, S, Ito, H, Traber, DL, Lee, JW, Cox, RA, Hawkins, HK, McAuley, DF, McKenna, DH, Traber, LD, Zhou, H, Herndon, Wilson, J, DN, Prough, DS, Matthay, MA and Enkhbaatar, P. Human Mesenchymal Stem Cells Reduce The Severity of Acute Lung Injury in an Ovine Model of Bacterial Pneumonia and Sepsis. Thorax 69(9):819-25, 2014.
- Ware, LB, Lee, JW, Wickersham, N, Nguyen, J, Matthay, MA, Calfee, CS and the California Transplant Donor Network. Donor smoking is associated with increased pulmonary edema and biomarkers of inflammation and lung epithelial dysfunction in the ex vivo donor lung. Am J Transplant 14(10):2295-302, 2014.
- Mar, JS, Nagalingam, NA, Song, Y, Onizawa, M, Lee, JW, and Lynch, SV. VSL#3 supplementation of mice is associated primarily with changes in ileal microbiota composition and amelioration of DSS-induced colitis. Gut Microbes 5(4):494-503, 2014.
- Liu, KD, Wilson, JG, Zhuo, H, Caballero, L, McMillan, M, Fang, X, Cosgrove, K, Calfee, CS, Lee, JW, Kangelaris, K, Gotts, J, Rogers, A, Levitt, J, Wiener-Kronish, J, DeLucchi, K, Leavitt, A, McKenna, D, Thompson, BT, Matthay, MA. Design and implementation of the START (STem cells for ARDS Treatment) trial, a phase 1/2 trial of human mesenchymal stem cells for the treatment of moderate-severe acute respiratory distress syndrome. Annals of Intensive Care 4:22, 2014.
- Wilson, JG, Liu, KD, Zhuo, H, Caballero, L, McMillan, M, Fang, X, Cosgrove, K, Vojnik, R, Calfee, CS, Lee, JW, Rogers, AJ, Levitt, J, Wiener-Kronish, J, Bajwa, EK, Leavitt, A, McKenna, D, Thompson, BT, Matthay, MA. Mesenchymal Stem (Stromal) Cells for Treatment of ARDS: A Phase 1 Clinical Trial. Lancet Rep Med 3:24-32, 2015.
- Kropski, JA, Pritchett, JM, Zoz, DF, Crossno, PF, Markin, C, Garnett, ET, Degryse, Al, Mitchell, DB, Polosukhin, VV, Rickman, OB, Choi, L, Cheng, DS, McConaha, ME, Jones, BR, Gleaves, LA, Worrell, JA, Solus, JF, Ware, LA, Stein, CM, Lee, JW, Massion, PP, Zaynagetdinov, R, White, ES, Johnson, JE, Groshong, SD, Lancaster, LH, Young, LR, Steele, MP, Phillips III, JA, Cogan, JD, Loyd, JE, Lawson, LE, Blackwell, TS. Extensive phenotyping of individuals at-risk for Familial Interstitial Pneumonia reveals clues to the pathogenesis of interstitial lung disease. AJRCCM 191:417-26, 2015.
- Wei, H, Zeng, Q, Zhang, F, Xue, Q, Luo, Y, Lee, JW, Cao, X, Yu, B, Feng, X. Ghrelin inhibits proinflammatory responses and prevents cognitive impairment in septic rats. Crit Care Med 43(5):e143-50, 2015.
- Gennai, S, Monsel, A, Hao, Q, Park, J, Matthay, MA, Lee, JW. Microvesicles Derived From Human Bone Marrow Mesenchymal Stem Cells Restored Alveolar Fluid Clearance in Marginal Donor Human Lungs Not Used For Clinical Transplantation. Am J Transplant 15(9):2404-12, 2015.
- Monsel, A, Zhu, YG, Gennai, S, Hao, Q, Hu, S, Rouby, JJ, Rosenzwajg, M, Matthay, MA, Lee, JW. Microvesicles Derived from Human Bone Marrow Mesenchymal Stem Cells Improve Survival in E.coli Pneumonia-induced Acute Lung Injury in Mice and Enhance Monocyte Phagocytosis of Bacteria. AJRCCM 192(3):324-36, 2015.
- Hao, Q, Zhu, YG, Monsel, A, Gennai, S, Lee, T, Xu, F, Lee, JW. Comparison of bone marrow and embryonic stem cell-derived human mesenchymal stem cells for treatment of E.coli Endotoxin-induced acute lung injury in mice. Stem Cells Transl Med 4(7):832-40, 2015.
- Prakash, A, Sundar, SV, Casbon , AJ, Zhu, YG, Tran, A, Lee, JW, Lowell, C, and Hellman, J. Lung Ischemia Reperfusion (IR) is a Transient Sterile Inflammatory Process Influenced by Commensal Microbiota. SHOCK 44(3):272-9, 2015.
- Fang, X, Abbott, J, Cheng, L, Colby, J, Lee, JW, Levy, B, Matthay, MA. Mesenchymal Stem Cells Promote Resolution of Lung Injury by Lipoxin A4. J Immunol 195(3):875-81, 2015.
- Rajasekaran, S, Tamatam, CR, Fang, J, Potteti, HR, Raman, V, Lee, JW, Matthay, MA, Mehta, D, Reddy, DM, and Reddy, SP. Visualization of Fra-1/AP-1 activation during LPS-induced inflammatory lung injury using fluorescence optical imaging. Am J Physiol Lung Cell Mol Physiol 309(4):L414-24, 2015.
- Du, R, Richmond, B, Blackwell, ST, Cates, JM, Massion, PP, Ware, LB, Lee, JW, Kononov, AV, Lawson, WE, Blackwell, TS, Polosukhin, VV. Secretory IgA From Tracheobronchial Submucosal Glands Does Not Compensate for its Surface Deficiency in Small Airways in Chronic Obstructive Pulmonary Disease. Virchows Archive 467(6):657-665, 2015.
- Chan, MCW, Kuok, DIT, Leung, CYH, Hui KPY, Valkenburg, SA, Lau, EHY, Nicholls, JM, Fang, X, Guan, Y, Lee, JW, Chan, RWY, Webster, RG, Matthay, MA, and Malik, JS. Human mesenchymal stromal cells reverse influenza A H5N1 associated acute lung injury in vitro and in vivo. PNAS 113(13):3621-6, 2016.
- Gordon ED, Palandra J, Wesolowska-Andersen A, Ringel L, Rios CL, Lachowicz-Scroggins ME, Sharp LZ, Everman JL, MacLeod HJ, Lee JW, Mason RJ, Matthay MA, Sheldon RT, Peters MC, Nocka KH, Fahy JV, Seibold MA. IL1RL1 asthma risk variants regulate airway type 2 inflammation. JCI Insight. 2016 Sep 8; 1(14):e87871. PMID: 27699235
- Fernandez-Bustamante, A, Frendl, G, Sprung, J, Kor, D, Subramaniam, B, Martinez Ruiz, R, Lee, JW, Henderson, W, Moss, A, Mehdiratta, N, Colwell, MM, Bartels, K, Kolodzie, K, Vidal Melo, M; The Perioperative Research Network (PRN) investigators. Multicenter prospective evaluation of postoperative pulmonary complications in non-cardiothoracic surgical patients with severe systemic disease. JAMA Surgery 2016 In Press.
- Liu, J, Kuwabara, A, Kamio, Y, Hu, S, Park, J, Hashimoto, T, Lee, JW. Human mesenchymal stem cell-derived microvesicles prevent the rupture of intracranial aneurysm in part by suppression of mast cell activation via a PGE2-dependent mechanism. Stem Cells 2016 In Press.
- Macrophage-derived microvesicles' pathogenic role in acute lung injury. Thorax. 2016 11; 71(11):975-976.
- IL1RL1 asthma risk variants regulate airway type 2 inflammation. JCI Insight. 2016 09 08; 1(14):e87871.
- Concise Review: Mesenchymal Stem (Stromal) Cells: Biology and Preclinical Evidence for Therapeutic Potential for Organ Dysfunction Following Trauma or Sepsis. Stem Cells. 2017 02; 35(2):316-324.
- Postoperative Pulmonary Complications, Early Mortality, and Hospital Stay Following Noncardiothoracic Surgery: A Multicenter Study by the Perioperative Research Network Investigators. JAMA Surg. 2017 02 01; 152(2):157-166.
- Secretory IgA Deficiency in Individual Small Airways Is Associated with Persistent Inflammation and Remodeling. Am J Respir Crit Care Med. 2017 04 15; 195(8):1010-1021.
- Protective Effect of Mesenchymal Stem Cells Against the Development of Intracranial Aneurysm Rupture in Mice. Neurosurgery. 2017 Dec 01; 81(6):1021-1028.
- Hu S, Park J, Liu A, Lee J, Zhang X, Hao Q, Lee, JW. Mesenchymal Stem Cell Microvesicles Restore Protein Permeability Across Primary Cultures of Injured Human Lung Microvascular Endothelial Cells. Stem Cells Transl Med. 2018 08; 7(8):615-624.
- Lee, JW, Kato H. Should We Stop for Growth Arrest-specific 6 in Acute Respiratory Distress Syndrome? Anesthesiology. 2018 07; 129(1):8-10.
- Park J, Kim S, Lim H, Liu A, Hu S, Lee J, Zhuo H, Hao Q, Matthay MA, Lee, JW. Therapeutic effects of human mesenchymal stem cell microvesicles in an ex vivo perfused human lung injured with severe E. coli pneumonia. Thorax. 2019 01; 74(1):43-50.
- Queiroz VNF, da Costa LGV, Barbosa RP, Takaoka F, De Baerdemaeker L, Cesar DS, D'Orto UC, Galdi JR, Gottumukkala V, Cata JP, Hemmes SNT, Hollman MW, Kalmar A, Moura LAB, Mariano RM, Matot I, Mazzinari G, Mills GH, Posso IP, Teruya A, Vidal Melo MF, Sprung J, Weingarten TN, Treschan TA, Koopman S, Eidelman L, Chen LL, Lee, JW, Ariño Irujo JJ, Tena B, Groeben H, Pelosi P, de Abreu MG, Schultz MJ, Serpa Neto A. International multicenter observational study on assessment of ventilatory management during general anaesthesia for robotic surgery and its effects on postoperative pulmonary complication (AVATaR): study protocol and statistical analysis plan. BMJ Open. 2018 08 23; 8(8):e021643.
- Lee JH, Park J, Lee, JW. Therapeutic use of mesenchymal stem cell-derived extracellular vesicles in acute lung injury. Transfusion. 2019 02; 59(S1):876-883.
- Lee, JW, Matthay MA. Is a Part Better than the Whole for Cell-based Therapy for Acute Respiratory Distress Syndrome? Anesthesiology. 2019 May; 130(5):683-685.
- Ross JT, Nesseler N, Lee, JW, Ware LB, Matthay MA. The ex vivo human lung: research value for translational science. JCI Insight. 2019 06 06; 4(11).
- Hao Q, Gudapati V, Monsel A, Park JH, Hu S, Kato H, Lee JH, Zhou L, He H, Lee, JW. Mesenchymal Stem Cell-Derived Extracellular Vesicles Decrease Lung Injury in Mice. J Immunol. 2019 10 01; 203(7):1961-1972.
- Abreu SC, Rolandsson Enes S, Dearborn J, Goodwin M, Coffey A, Borg ZD, Dos Santos CC, Wargo MJ, Cruz FF, Loi R, DeSarno M, Ashikaga T, Antunes MA, Rocco PRM, Liu KD, Lee, JW, Matthay MA, McKenna DH, Weiss DJ. Lung inflammatory environments differentially alter mesenchymal stromal cell behavior. . 2019 12 01; 317(6):L823-L831.
- Liu A, Park JH, Zhang X, Sugita S, Naito Y, Lee JH, Kato H, Hao Q, Matthay MA, Lee, JW. Therapeutic Effects of Hyaluronic Acid in Bacterial Pneumonia in Ex Vivo Perfused Human Lungs. Am J Respir Crit Care Med. 2019 11 15; 200(10):1234-1245.
- Liu A, Zhang X, He H, Zhou L, Naito Y, Sugita S, Lee, JW. Therapeutic potential of mesenchymal stem/stromal cell-derived secretome and vesicles for lung injury and disease. Expert Opin Biol Ther. 2020 02; 20(2):125-140.
- Lee JH, Liu A, Park JH, Kato H, Hao Q, Zhang X, Zhou L, Lee, JW. Therapeutic Effects of Hyaluronic Acid in Peritonitis-Induced Sepsis in Mice. Shock. 2020 10; 54(4):488-497./li>
- Proinflammatory cytokines and ARDS pulmonary edema fluid induce CD40 on human mesenchymal stromal cells-A potential mechanism for immune modulation. PLoS One. 2020; 15(10):e0240319.
- Ventilation and outcomes following robotic-assisted abdominal surgery: an international, multicentre observational study. Br J Anaesth. 2021 02; 126(2):533-543.
- Baljinnyam T, Radnaa E, Ouellette CM, Nelson C, Niimi Y, Andersen CR, Popov V, Lee, JW, Prough DS, Enkhbaatar P. High molecular weight sodium hyaluronate improves survival of syndecan-1-deficient septic mice by inhibiting neutrophil migration. PLoS One.. 2021; 16(4):e0250327.
- Zhou L, Hao Q, Sugita S, Naito Y, He H, Yeh CC, Lee, JW. Role of CD44 in increasing the potency of mesenchymal stem cell extracellular vesicles by hyaluronic acid in severe pneumonia.Stem Cell Res Ther. 2021 May 20; 12(1):293.
- Gutor SS, Richmond BW, Du RH, Wu P, Sandler KL, MacKinnon G, Brittain EL, Lee, JW, Ware LB, Loyd JE, Johnson JE, Miller RF, Newman JH, Rennard SI, Blackwell TS, Polosukhin VV. Postdeployment Respiratory Syndrome in Soldiers With Chronic Exertional Dyspnea. Am J Surg Pathol.. 2021 Jun 03.
- Naito Y, Kato H, Zhou L, Sugita S, He H, Zheng J, Hao Q, Sawa T, Lee JW. Therapeutic Effects of Hyaluronic Acid Against Cytotoxic Extracellular Vesicles Released During Pseudomonas Aeruginosa Pneumonia. Shock. 2021 Aug 13.
- Zeng C, Lagier D, Lee JW, Vidal Melo MF Perioperative Pulmonary Atelectasis: Part I. Biology and Mechanisms. Anesthesiology, 2021 Sep 08.
- Zhang X, Sugita S, Liu A, Naito Y, Hwang W, Qiu H, Sakamoto A, Sawa T, Matthay MA, Lee JW. Therapeutic Effects of High Molecular Weight Hyaluronic Acid in Severe Pseudomonas Aeruginosa Pneumonia in Ex Vivo Perfused Human Lungs. Am J Physiol Lung Cell Mol Physiol, 2021 09 15.
- Gutor SS, Richmond BW, Du RH, Wu P, Sandler KL, MacKinnon G, Brittain EL, Lee JW, Ware LB, Loyd JE, Johnson JE, Miller RF, Newman JH, Rennard SI, Blackwell TS, Polosukhin VV, Gutor SS, Richmond BW, Du RH, Wu P, Sandler KL, MacKinnon G, Brittain EL, Lee JW, Ware LB, Loyd JE, Johnson JE, Miller RF, Newman JH, Rennard SI, Blackwell TS, Polosukhin VV. Postdeployment Respiratory Syndrome in Soldiers With Chronic Exertional Dyspnea. Am J Surg Pathol, 2021 12 01; 45(12):1587-1596.
- Zeng C, Lagier D, Lee JW, Vidal Melo MF, Zeng C, Lagier D, Lee JW, Vidal Melo MF. Perioperative Pulmonary Atelectasis: Part I. Biology and Mechanisms. Anesthesiology, 2022 01 01; 136(1):181-205.
- Naito Y, Kato H, Zhou L, Sugita S, He H, Zheng J, Hao Q, Sawa T, Lee JW, Naito Y, Kato H, Zhou L, Sugita S, He H, Zheng J, Hao Q, Sawa T, Lee JW. Therapeutic Effects of Hyaluronic Acid Against Cytotoxic Extracellular Vesicles Released During Pseudomonas Aeruginosa Pneumonia. Shock, 2022 03 01; 57(3):408-416.
- Hwang W, Shimizu M, Lee JW. Role of extracellular vesicles in severe pneumonia and sepsis. Expert Opin Biol Ther. 2022 Apr 14.
- Bartels K, Frendl G, Sprung J, Weingarten TN, Subramaniam B, Martinez Ruiz R, Lee JW, Henderson WG, Moss A, Sodickson A, Giquel J, Vidal Melo MF, Fernandez-Bustamante A, Perioperative Research Network (PRN) investigators. Postoperative pulmonary complications with adjuvant regional anesthesia versus general anesthesia alone: a sub-analysis of the Perioperative Research Network study. BMC Anesthesiol. 2022 May 03; 22(1):136
- Gutor SS, Richmond BW, Du RH, Wu P, Lee JW, Ware LB, Shaver CM, Novitskiy SV, Johnson JE, Newman JH, Rennard SI, Miller RF, Blackwell TS, Polosukhin VV. Characterization of Immunopathology and Small Airway Remodeling in Constrictive Bronchiolitis. Am J Respir Crit Care Med. 2022 May 13
- Zhou L, Luo H, Lee JW. Role of extracellular vesicles in lung diseases. Chin Med J (Engl). 2022 Jul 25
REVIEW ARTICLES/CHAPTERS/EDITORIALS:
- Monsel, A, Zhu, YY, Hao, Q, Liu, J, Gennai, S, and Lee, JW. Cell-based Therapy for Acute Organ Injury: Preclinical Evidence and On-going Clinical Trials Using Mesenchymal Stem Cells. Anesthesiology 121(5):1099-121, 2014.
- Gennai, S, Monsel, A, Hao, Q, Liu, J, Gudapati, V, and Lee, JW. Cell-Based Therapy for Severe Traumatic Brain Injury. British J Anesth 115 (2): 203–12, 2015.
- Lee, JW, Rocco, P, Pelosi, P. Mesenchymal Stem Cell Therapy for Acute Respiratory Distress Syndrome: A Light at the End of the Tunnel? Anesthesiology 122:238-40, 2015. Editorial.
- Monsel, A, Zhu, YG, Gudapati, V, Lim, H, and Lee, JW. Mesenchymal Stem Cell Derived Extracellular Vesicles for Acute Lung Injury. Expert Opinion in Biological Therapy 16(7):859-71, 2016.
- Monsel, A, Zhu, YG, Gudapati, V, and Lee, JW. Treatment of lung disease by MSC microvesicles (exosomes). Chapter in, The Biology and Therapeutic Application of Mesenchymal Cells. Ed. Kerry Atkinson. John Wiley Publishers Inc. Hoboken, New Jersey, USA. 2016.
- Matthay, M, Pati, S, and Lee, JW. Therapeutic Role of Mesenchymal Stem Cells in Organ Injury. Stem Cells 2016, In Press.
- Lee, JW. Macrophage-derived microvesicles pathogenic role in acute lung injury. Thorax, 2016. Editorial. In Press.
Jae-Woo Lee, MD
Principle Investigator
Associate Professor of Anesthesiology, UCSF
Qi Hao, PhD
Dr. Hao is studying the therapeutic use of microvesicles released by preconditioned mesenchymal stem cells to express pro-apoptotic agents for treatment of metastases from breast cancer in NOD/SCID mice in collaboration with Dr. Sam M. Janes (University College London, UK).
Antoine Monsel, MD
Visiting Scholar
La Pitié-Salpétrière Hospital, Paris, France
Dr. Monsel is studying the therapeutic use of microvesicles released by preconditioned mesenchymal stem cells in small animal models of severe bacterial pneumonia.
Stephane Gennai, MD
Visiting Scholar
Grenoble University Hospital, Grenoble, France
Using a novel ex vivo perfused human lung preparation, Dr. Gennai is studying the therapeutic use of microvesicles released by preconditioned mesenchymal stem cells in reconditioning human lungs declined for transplantation in collaboration with Dr. Michael A. Matthay (UCSF).
For individuals interested in post-doctoral positions, please contact:
Jae-Woo Lee, MD
UCSF Medical Center
Department fo Anesthesiology
505 Parnassus Ave, Box 0648
[email protected]
Phone: (415) 476-0452