From the April 2018 UCSF Department of Medicine, Pulmonary, Critical Care, Allergy and Sleep Medicine Division Newsletter - Clinical Program Highlight:
Ten month wait times, frustrated referring providers, and indefensibly poor patient satisfaction. Increasing referral volume and fixed limits to testing capacity. These describe the operational realities of the ZSFG Sleep Program in 2014. Our program struggled despite generous support from David Claman, MD, and the UCSF Sleep Disorders Center, dutiful study interpretation and reporting from our fellows and faculty, and heroic efforts of ZSFG PCCM Administrator Mary DeJesus and ZSFG Respiratory Care Services sleep lead Mark Siobal, RRT. Our plight then, was to rescue our program—and to do so with little chance of expanding site testing or personnel resources, and zero chance for positive revenue streams given our largely Med-Cal managed-care constituency.
In 2015, supported by seed funding from the California HealthCare Foundation (CHCF), we re-imagined and re-designed the ZSFG Sleep Program. We configured a unique public-private collaborative arrangement with a local sleep testing laboratory, retained professional fee reimbursements by interpreting all studies, discontinued ZSFG on-site polysomnogram (PSG) testing, shifted the primary testing offering for high-likelihood obstructive sleep apnea (OSA) to home sleep testing (HST), and brought on Eula Lewis RRT (sponsored by ZSFG Director of Respiratory Care Services John Kelly RRT) and ZSFG PCCM nurse specialist Stephanie Tsao NP to elevate our delivery of patient-centered care. Our testing model, heavily scrutinized, and ultimately approved by our system’s major Medi-Cal provider (San Francisco Health Plan (SFHP)) incorporates questionnaire-based referral support, attending-level adjudication of electronic referrals by ZSFG PCCM faculty Christina Yoon MD and Adithya Cattamanchi MD, and final order placement by a board-certified sleep specialist. A business plan outlining budget support for this new program structure was submitted to and approved by the City of San Francisco.
Within 3 months of our new program rollout, study wait times dropped 83% to 7 weeks. Current next-available appointments remain stable at <4 weeks for PSGs and <2 weeks for HSTs. The testing backlog of 250 patients has been reduced to zero. We service over 500 HSTs and over 400 PSGs per year, effectively increasing our testing capacity by 270% since 2014. Our ZSFG PCCM fellows and faculty perform all study interpretations. Our program now features a new ZSFG Sleep Clinic, a standalone ZSFG Respiratory Therapy Sleep Clinic to address problems related to positive airway pressure (PAP) use, and “The Good Night” OSA group patient education course.
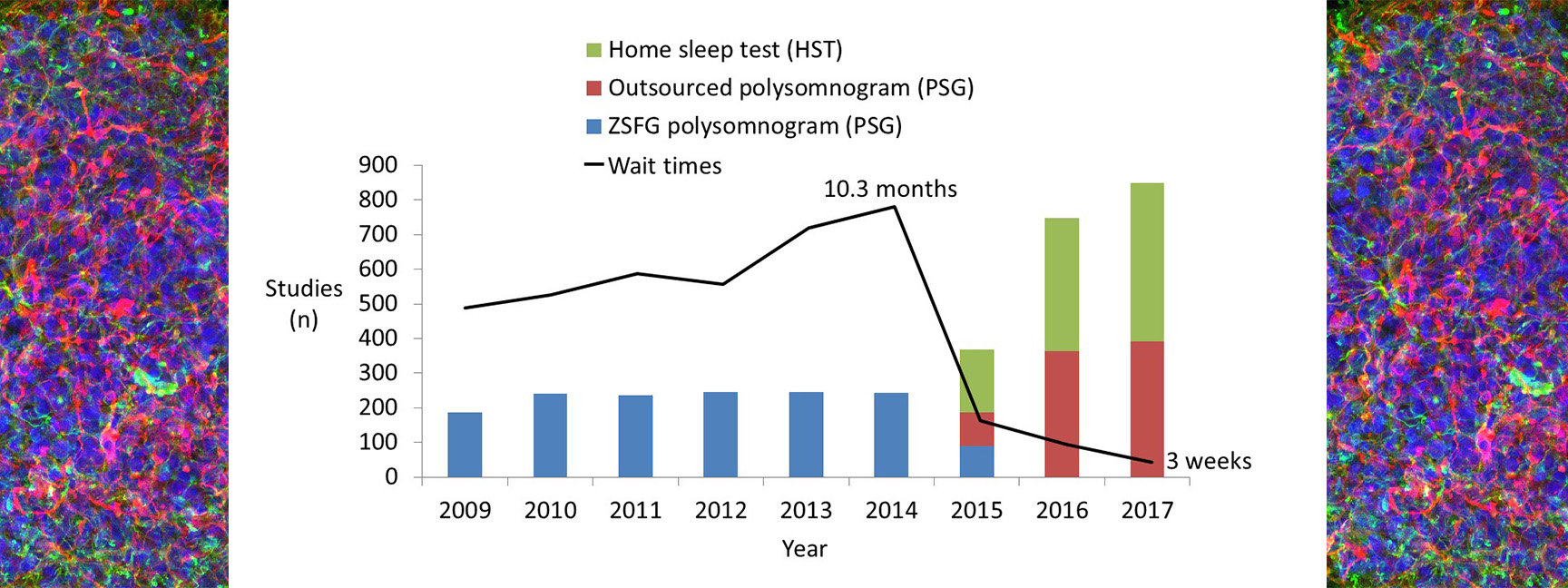 Figure: ZSFG Sleep Program Study Volume and Wait Times
Figure: ZSFG Sleep Program Study Volume and Wait Times
We are now focused on enhancing the educational offerings and value to our PCCM fellows by increasing fellow exposure to care for sleep-disordered breathing and a wider array of sleep disorders in both our ZSFG Chest continuity and Sleep Clinics, and by improving HST interpretation support. Operationally we look to adopt video-enabled encounters to promote better access to provider services, and seek to tackle the formidable challenge of poor PAP adherence by leveraging data, artificial intelligence, and predictive analytics.
Our current program members include George Su MD (medical director), Mary DeJesus, Eula Lewis RRT CTTS AE-C, Stephanie Tsao NP, Myron Fong RRT, Christina Zepeda MEA, and Katie O’Shea (ZSFG PCCM analyst).
